Immune Strategies for Cancer Treatment
In the search for innovative and effective ways to target cancer, we are faced with more than just a challenging problem; we are faced with our own cells as opponents. Cancer cells evolve to achieve an optimum of physical fitness, giving them an array of abilities that no cell should possess in a healthy organism. One way to find novel therapies against cancer therefore could imply finding a solution that counterbalances centuries of evolution towards enhanced physical fitness in our very own cells. Notwithstanding constantly changing convictions on ideal cancer therapies, there is a consensus that fighting cancer requires aggressive therapies. Bold cancer therapies have come in different forms since the early 20th century and have transitioned from mostly macroscopic but local procedures to more microscopic, systemic therapies, for example in the form of chemotherapies, or more recently, immunotherapies. Immunotherapies harness the power of our immune system to better target and eliminate tumors; why is this an attractive option? What are the challenges? What solutions have been engineered so far?
Overview of the Immune System
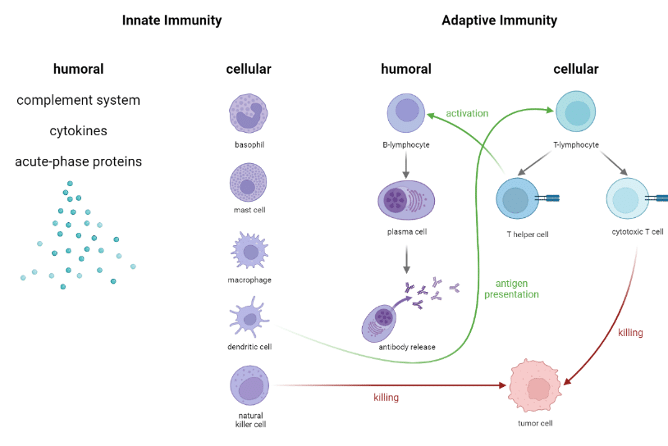
The immune system is made of an infinitely complex array of cells and molecules that work together to recognize and eliminate pathogens, foreign elements, but also cancer cells. The immune system was optimized over the course of centuries of evolution, and it is our greatest weapon against cancer. For many years, research focused mainly on immune response to cancer. This research has enabled a far better understanding of the key players in cancer immunology; now, the acquired knowledge can be used to better target. Below is an overview of the main players in the immune system, showing selected synergies amongst various cell types. As seen in the graph below, some cells play a more central role than others; T helper cells for example are a key link between the cellular adaptive response and the humoral adaptive response (you can find out more about T helper cells in our blog post about HIV), while other immune cells have cytotoxic effects such as natural killer (NK) or some T cells. So which cells are best used for immunotherapies?
Immune Checkpoint Inhibitors
Controlling the strength and amplitude of an immune response is a critical feature of a healthy immune system. Dysregulation of this can cause a myriad of problems such as autoimmune diseases; there are therefore several mechanisms by which immune cell effector functions are kept under control to limit exaggerated responses. One such mechanism are the so-called “immune checkpoints”: these are molecules found on the surface of T cells. When a cell binds both the T-cell receptor (the receptor specific for a given antigen, that gives a T cell its specificity) and the checkpoint molecule (PD-1 in the displayed figure), the T cell becomes inactivated. Tumors utilize this and express the binding partner to immune checkpoint molecules; by doing so, they inhibit T cell function when a T-cell recognizes them and hide from the immune system (a phenomenon termed “immune evasion”). Drugs such as the anti PD-1 antibody bind immune checkpoint molecules on T cells, so that cancer cells cannot bind them to inhibit T cell function.
These drugs have shown some success; the caveat is that while immune cell function is no longer hampered with regards to cancer cells, it is not targeted to tumor-specific T cells. This means that T cell function can no longer be controlled by checkpoint molecules, which can cause highly exaggerated immune responses and drastic side-effects.
CAR T Cell Therapy
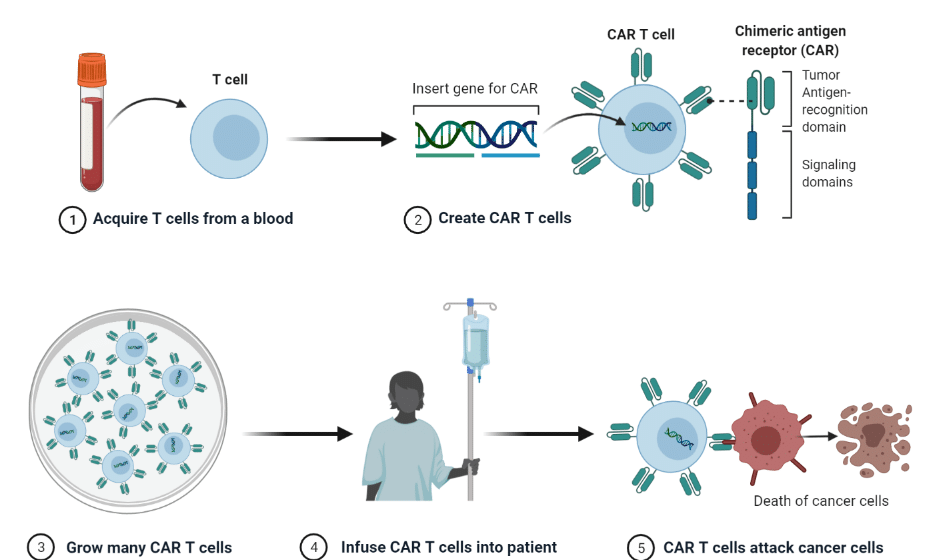
CAR T cell therapy is another immunotherapy utilizing cytotoxic T cells. In this approach, a patient’s T cells are extracted and purified from a blood sample; they are subsequently genetically modified to express a T-cell receptor specific to a tumor antigen unique to the patient’s cancer cells. This receptor is called “chimeric antigen receptor”, or CAR. Once the modified T cells are made, they are amplified to reach sufficient numbers, and reinjected into the patient. The engineered T cells (CAR T cells) then specifically recognize the cancer cells and eliminate them.
CAR T cell therapy has had tremendous success for certain cancer types, such as leukaemia. However, solid tumors have been more difficult to address with this approach, as tumor cells have found ways to evade CAR T cell functions as well, making the therapy less effective and less durable. Many strategies are being tested to solve this issue, including creating bi- or tri-specific CARs to recognize multiple tumor antigens simultaneously, or conjugating CAR T cells with other drugs. Nevertheless, CAR T cell therapy still shows much promise, and is a highly researched field.
Dendritic Cell Vaccine
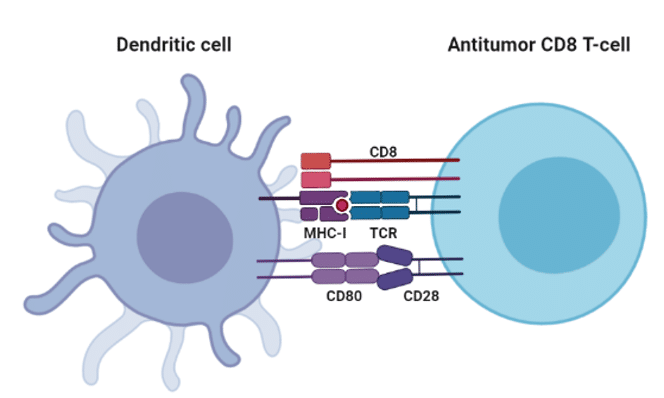
Not all immunotherapies focus on T cells; other immune cells can be harnessed for anti-cancer effects. One such candidate is the dendritic cell (DC), one of the most powerful and polyvalent cells in the immune system. DCs have several functions in the immune system depending on their level of maturity: mature DCs are mainly responsible for antigen presentation to T cells, giving DCs the common categorization of “antigen-presenting cells”. As such, they present antigens to T cells, which initiates a T cell response.
Utilizing DCs is therefore an indirect way to control T cell function. One idea was to utilize this feature and develop a dendritic cell vaccine against a tumor. By extracting immature dendritic cells from a patient, priming them to express a given tumor antigen, and then reinjecting them into the patient once they have matured, the DCs then present the desired tumor antigen to T cells, which can then develop into cytotoxic T cells capable of killing cancer cells, but also memory cells against this antigen, should the tumor begin to spread again (hence the DC “vaccine”).
This strategy has shown only little clinical success, and significantly less than T cell-based immunotherapies. DCs are also quite rare cells, and difficult to culture, making their manufacturing challenging and not as suitable for industrial production as other immune cells.
Conclusion
This article gave some insight on the highly researched topic of immunotherapies; this growing field is striving towards novel solutions for better, more efficient, and more durable cancer therapies. Much work still must be done to address their current shortcomings, such as their side-effects and the observed immune evasion still seen in solid tumors, but immunotherapies are currently the most promising technologies for cancer treatment.
References
https://www.nature.com/articles/d42859-020-00022-7
Biorender.com
GeoWissen


